Fibroid Surgery - Procedure, Types, Benefits & Recovery

Treatment Duration
45 Minutes
------ To ------55 Minutes
Treatment Cost
₹ 40,000
------ To ------₹ 1,20,000

Table of Contents
You can check Fibroid Removal Surgery (Open Myomectomy) Cost here.
About
Why Is Myomectomy Done?
Myomectomy is done to remove fibroids from the uterus. Most small fibroids do cause any symptoms and do not require any treatment except regular observation by your doctor. However, larger fibroids can cause a variety of symptoms and may need myomectomy. These symptoms include:
- Difficulty in getting pregnant: If you have a fibroid that has changed the uterus walls and can cause infertility, myomectomy is done to improve the chances of pregnancy before in-vitro fertilisation.
Myomectomy is a procedure that will enhance your chances of having a baby. It is because it helps to remove a certain kind of fibroid called submucosal fibroid (growths located under the mucosal layer). Myomectomy preserves the uterus and only extracts the fibroids.
- Excessive painful bleeding during your periods
- Frequent urination, which can happen when a fibroid puts pressure on your uterus.
- Bleeding between the periods
- Lower back pain and constipation, along with all the other symptoms
- The inability to empty your bladder completely; a feeling of fullness in your lower abdomen.
- Your abdomen is distended, making you look pregnant.
It can also happen that symptoms of these fibroids either stabilise or go away when you have gone through menopause. This occurs because the hormone levels decline in your body after menopause.
Figure: Uterine Fibroids
When to See a Doctor?
You should seek your doctor if you observe the following symptoms of uterine fibroids:
- Pelvic pain
- Pregnancy problems
- Infertility
- Frequent urination
- Heavy and extended bleeding in your periods
- Constipation
- Bloating.
- Dysmenorrhea (Painful menstrual periods, accompanied by uterine contractions).
- Menorrhagia (Menstrual periods with abnormally lengthy periods).
- Metrorrhagia (Uterine bleeding at irregular intervals).
- Abnormal uterine bleeding.
- Dyspareunia (pain during sexual intercourse).
If you have minor signs and symptoms, your doctor may recommend other treatments, such as hormone therapy or pain medicines. A myomectomy will only remove the fibroids, and the uterus will be left in place. This reason makes it an appropriate option for women who want to have a baby.
What to Expect if You Delay Surgery?
If your uterine fibroids go untreated, you can expect severe outcomes, such as:
- Severe anaemia
- Extensive bleeding after childbirth or surgery
- Lower quality of life
- Arthritis and breakdown of joints.
- Bleeding in other areas of the body.
- Development of uterine myomas.
- Infertility
- Maternal and fetal related pregnancy complications
- Significant morbidity is seen if uterine fibroids are left untreated.
Fibroid Removal Surgery (Open Myomectomy) Videos by HexaHealth
Expert Doctors (10)
NABH Accredited Hospitals (10)


Procedure Description
There are two ways in which a myomectomy can be performed:
Open myomectomy:
- It is also called an abdominal myomectomy.
- This procedure is chosen for extremely large fibroids.
- An incision is made in your abdomen. This incision can go across the bikini cut, or it can go up and down.
- The fibroids are then removed from the walls of the uterus.
- The uterine muscle is then sewn back together using several layers of stitches.
Minimally invasive myomectomy:
There are many types of minimally invasive options for a myomectomy. These surgeries usually have faster recovery rates and are easier on your body.
1. Standard Laparoscopic Myomectomy:
Several minor cuts are made in the abdomen to place instruments needed to move fibroids in this surgery.
- One of those instruments is a small telescope that is inserted through the belly button.
- The fibroids are then removed through small incisions or sometimes through the vagina.
- The surgeon may opt to get the aid of a robot, to finely control the movements of instruments in this type of surgery.
2. Single Port Myomectomy:
- Unlike laparoscopic myomectomy, this procedure uses only one opening near the belly button for all the instruments.
- This results in a slightly larger incision or a scar after the surgery, but there are no other incisions on the abdominal wall.
3. Hysteroscopic Myomectomy:
- No incision is made in this type of surgery.
- When the fibroids are in the right place inside the uterus, the surgeon places a specialised camera through the vagina.
- This camera has an attachment to remove the fibroids directly from the vagina.
For all the surgeries, when the procedure is completed, the instruments will be removed. If any incisions, they will be closed and bandaged.
What to Plan Before Surgery?
Before the surgery, your doctor will make sure of the treatment that is best suitable for you. It will depend upon:
- Your signs and symptoms
- The position, size, and a number of the fibroids in your uterus.
- Your future desires, if you want to get pregnant in the future or preserve your uterus for any other reasons.
If your doctor has chosen myomectomy as a treatment for you, some decisions are still to be made. They may include the decision of the type of myomectomy to be performed. It will depend upon various factors, including:
- Fibroid size
- The number of fibroids
- The experience of the surgeon
- The position of fibroids in the uterus.
Before the surgery, tell your doctor about the medicines you take, including over-the-counter medications such as aspirin. Also, inform them about other prescription medicines such as vitamins, herbs, and other supplements. Some medicines, such as blood thinners, may need to be stopped before the surgery.
Diagnosis:
Before the surgery, your surgeon will ask for several diagnostic tests to determine the fibroids' size, location, and number.
A uterine fibroid can be diagnosed with several tests, such as:
- Physical test: The fibroids can be felt by your doctor during a regular pelvic exam. To confirm and to determine their exact location, other tests need to be done.
- Ultrasonography: This procedure creates a picture of your internal organs using sound waves. Depending upon the size of the uterus, this ultrasound may be carried out via transvaginal (through the vagina) or transabdominal (through the abdomen) route.
- Magnetic resonance imaging (MRI): This procedure uses magnets and radio waves to create detailed images of your internal organs.
- Computed tomography (CT): X-ray images are taken through a CT scan through various angles.
- Hysteroscopy: To look at fibroids inside your uterus, a hysteroscopy uses a device called a scope. This device has a thin, long tube with a tiny camera attached to it. A scope passes through your vagina and cervix and then moves into your uterus to take pictures.
- Hysterosalpingography (HSG): A contrast material is injected inside the uterus at first, and then detailed X-rays of the uterus are taken.
- Sonohysterography: This procedure provides more precise images than a standard ultrasound. This is an imaging test, and a catheter is placed transvaginally. Saline is inserted through that catheter. The extra fluid from the saline helps to create a clearer image.
- Blood tests: blood tests are done to check for anaemia and infection and to look at kidney function.
You will meet your anesthesiologist a few days prior to the procedure for the following
- Your medical history (including anaesthesia history) will be checked, and the results of the investigations advised by your doctor will be reviewed.
- Based on the discussion, the anesthesiologist will decide the type of anaesthesia you will need.
- General anaesthesia is preferred in surgeries of the upper body.
- You need to prevent yourself from consuming solid foods for at least six hours and water at least two hours before the surgery. Anaesthesia temporarily stops your body's reflexes. If you have food in your stomach and you vomit or bring up food while under the effect of anaesthesia, the food can enter your lungs and cause damage to the lungs. Your stomach should be empty to prevent this.
You may be asked to be admitted to the hospital a few hours or the night before the surgery if specific tests need to be performed before the surgery.
On the Day of Surgery:
In the Preoperative room, where you can expect the following:
- The anesthesiologist will go through your pre-anaesthesia check-up reports to confirm that you are fit for surgery.
- Wear a hospital gown, will be provided with an identity bracelet and allergy bracelet on your wrist that will have your name and the name of the hospital on it.
- The healthcare staff will ask you to remove your clothing, jewellery, glasses, hairpins, contact lenses or any objects that may interfere with the surgery. Dentures and loose teeth also need to be removed prior to the surgery to prevent any dental damage or risks.
- The healthcare staff will note the following information:
- The time of your last meal and fluids.
- Medical history, current symptoms and allergies.
- Monitor the vital signs
- The healthcare staff will trim the hair on the surgical site if needed.
- They will place a soft, thin tube called an intravenous line into a vein in your hand or arm so that medicines can be given directly into your blood vessel.
What to Expect During Surgery?
- In the Operative room,
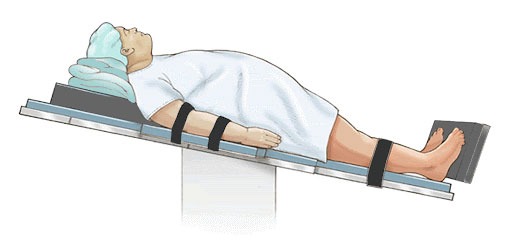
- You will be positioned in the 10-degree reverse Trendelenburg position, as shown in the figure below.
- You will receive the medicine for general anaesthesia through the intravenous line. In some cases, anaesthesia will be administered through a breathing mask. If you receive anaesthesia via a breathing mask, the anaesthetic agent will be mixed with oxygen.
- As soon as you are given general anaesthesia, you will begin to feel light-headed and lose consciousness within a minute.
- After the surgery is completed, a sterile bandage will be applied
What to Expect After Surgery?
At Hospital:
You will be shifted from the operating room to the recovery room (also called the postoperative room) where:
- The healthcare staff will closely monitor your condition for a few hours.
- You will feel weak, cold, and confused after you wake up. All of these after-effects of anaesthesia usually subside in a few hours.
- You will be asked not to drink anything until you have fully recovered from anaesthesia; this usually takes about four hours and depends on the nature of the surgery.
- You will receive painkillers and antibiotics for post-surgical pain and prevent any infection, respectively.
- Urinary retention (unable to pass urine) can sometimes occur after being given anaesthesia
After completely recovering from anaesthesia:
- You will be moved to your allocated room or the ICU as needed. Ask the nurse if you can drink some water at this point, as per the orders given by your surgeon.
- If you have had outpatient surgery, you will be sent home on the same day after you are stable on monitoring. If you have had an inpatient surgery, you will stay at the hospital depending on the complexity of the surgery and postoperative recovery.
- The nurse will note any vaginal discharge.
- You may have some tubes at the surgical site to drain off excess fluid if necessary.
- Your catheter to drain off urine will be removed the following day or so.
- You should perform your breathing, coughing and leg exercises hourly.
At Home:
- You may get to go home that same day or need to stay overnight in the hospital. Then, when you're ready to go home, you'll need to have someone drive you.
- The hospital will provide you with essential pain medicines for your postoperative pain.
- You should resume a regular diet as soon as you are able to.
- To prevent the development of blood clots, moving around is recommended by doctors.
- Recovery time for an open myomectomy will be up to six weeks at home. For minimally invasive procedures like laparoscopic myomectomy, the recovery time is two to four weeks. However, recovery is just a matter of days if the surgery is done hysteroscopically (through the vagina without incisions).
- Depending on the type of procedure, you can return to work within two to six weeks (abdominal myomectomy takes the longest recovery time).
- After two weeks, you should aim to walk for about 10 minutes every day, unless advised otherwise by your doctor.
Risks & Complications
When to See a Doctor?
Consult your doctor for a follow-up appointment 4-6 weeks after the surgery. Additionally, see your doctor right away if you observe the following symptoms:
- You cannot pass stools or gas.
- You are unable to drink fluids and have an abnormal feeling in the stomach.
- Your incision is not closed because of loose stitches
- The bandage over your incision is soaked with bright red blood
- You have signs of infection, such as:
Increased swelling, warmth, pain, or redness
Discharge of pus from the incision
A fever - Excessive bleeding that soaks up more than one pad in an hour.
- Blood clots in your legs.
- Foul-smelling vaginal discharge.
More Treatment options
Last Updated on: 30 October 2023
Author
HexaHealth Care Team
HexaHealth Care Team brings you medical content covering many important conditions, procedures falling under different medical specialities. The content published is thoroughly reviewed by our panel of qualified doctors for its accuracy and relevance.
Fibroid Removal Surgery (Open Myomectomy) Cost in Top Cities
Other Treatments in Your City

























